The Peptamen® Junior formulae:
- Nutritionally complete with protein levels adapted to paediatric patients, contribute to meeting nutritional goals and enhance children's nutritional options1,2
- Uniquely provide hydrolysed 100% whey protein for improved nutrient absorption and gut function2-8
- Rich in medium-chain triglycerides (MCTs) to reduce fat malabsorption and improve overall tolerance9-13
- Clinically proven to improve health outcomes and growth1,2,13-19
- Well tolerated in children and can help reduce medication use1,2
Overall, with its enzymatically hydrolysed 100% whey protein and a high MCT content, the Peptamen® Junior portfolio provides convenient, high-performance delivery with a unique well-balanced protein and energy composition, while improving feeding tolerance and supporting a better quality of life.1,2
Peptamen® Junior range is our well-balanced peptide-based enteral feeding formulae.
When your paediatric patients suffer from a gastrointestinal disorder or disease, it is important to choose the right nutritional solution to help them throughout their journey and improve their quality of life.

Why is Peptamen® Junior made with hydrolysed 100% whey protein?
Whey protein:
- Is easy to digest2,5,20
- Allows for shorter gastric emptying time1, 7, 13, 14, 21
- Ensures fast delivery of amino acids and promotes normal growth and development3,4
- Improves nitrogen absorption and utilization5,13
- Contributes to maintaining gut health5
- Reduces episodes of vomiting, diarrhea and regurgitation1,7,13,14,22
Why does Peptamen® Junior contain medium-chain-triglycerides (MCTs)?
Medium-chain triglycerides (MCTs):
- Provide an easily available source of energy4
- Minimize fat malabsorption9,12,13
- Facilitate gastric emptying10,11
- Improve carbohydrate tolerance12,23
Learn more about the importance of WHEY PROTEIN and MCT
Why should you choose Peptamen® Junior?
Supported by more than 30 years of clinical experience and more than 20 clinical studies in paediatrics, Peptamen® Junior helps your patients recover rapidly with improved clinical outcomes.
Studies show that Peptamen® Junior helps in:14-19
- Reducing complications
- Shortening length of stay of patients in the intensive care unit (ICU)
- A faster recovery at the hospital or at home
Who can take Peptamen® Junior?
Peptamen® Junior can help a wide variety of paediatric patients along the continuum of care from enteral nutrition in the ICU to enteral feeding at home. Each product of the Peptamen® Junior range is tailored to specific needs. Assessment should be made based on energy needs and length of feeding required.
For example, children with reduced energy needs who suffer from a traumatic brain injury, a spinal cord injury or a neurological impairment with low mobility are recommended to take the Peptamen® Junior 0.6.
Discover our newest and most innovative formulae
Each child deserves an adapted formula. Learn about our 3 most innovative products to meet your patients' nutritional requirements, from low-energy to high-energy needs and high-fibre content.

Peptamen® Junior 0.6
For children with reduced energy requirements to avoid overfeeding
Weight management
- Mitigates the risks of overfeeding and excessive weight gain24-26
- Promotes weight stabilisation24
- Reduces the risk of developing other comorbities25
Tolerance and GI symptoms optimisation
- Optimises tolerance in tube-fed children with neurological impairment24
- Improves GI symptoms related to intolerance to feeds24,26
Practical and cost- and time-saving solution
- Eliminates the need for additional fluid, electrolytes and multivitamins, thereby reducing time and financial cost attributed to feeding24
Ready-
to-drink

Peptamen® Junior 1.5
For children with high energy needs who cannot tolerate polymeric oral nutritional supplementation (ONS)
Growth, weight gain and higher energy
- Supports improved growth, weight gain, and energy levels in children2,27
- 82% of children achieved their nutritional goals after switching to Peptamen® Junior 1.528
Digestion and tolerance
- Improves digestion and nutrient absorption2,7,27
- Helps decrease episodes of vomiting, retching, and gagging2,7,27,28
Flexible feeding options
- Can be used as oral supplement or bolus feed, providing flexibility for children with different feeding needs2
- Optimised nutritional intake without increasing the volume of the feed27
- Decreases feeding times, which leads to better quality of life for patients and their families2,27
High-fibre,
fully-
digestible

Peptamen® Junior PHGG
For children having diarrhoea, constipation, bowel mobility problems, gut pain, or discomfort
Nutrition
- One of the highest fibre contents among currently available paediatric enteral nutrition formulae
Tolerance and GI symptoms optimisation
- Is well tolerated29
- Gradual introduction of fibre may facilitate progressive GI adaptation and lessen risk for developing GI intolerance symptoms30
Stools
- Promotes colonic peristalsis31-35
- Facilitates defecation31-35
- Shifts towards softer and more frequent stools29
- May have a role in the clinical management of chronic constipation29
- May enable a reduction in laxative treatment in some patients29
Decision tree to help you identify right product according to your patients' needs
GI* impairment: Dysphagia / Gastro-oesophageal reflux disease (GORD) / Volume or fluid restrictions / Maldigestion / Malabsorption
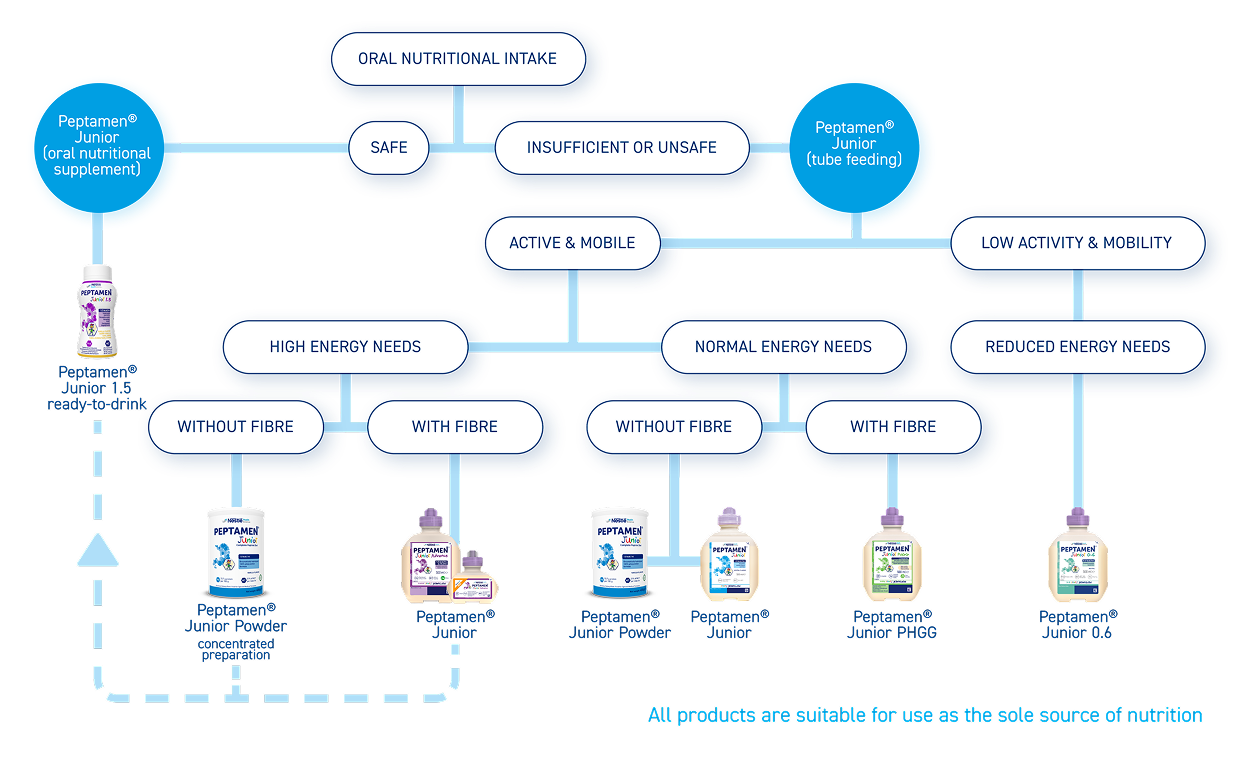
*GI, Gastrointestinal
Nutrition for Oral and Tube-Fed Patients
Identify the right product according to your patients’ needs
GI* impairment: Dysphagia/Gastro-oesochageal reflux disease (GORD)/Volume or fluid restrictions/Maldigestion/Malabsorption

PEPTAMEN® JUNIOR
(oral nutritional supplement)
PEPTAMEN® JUNIOR
(tube feeding)
References:
1.Minor G, et al. Glob Pediatr Health 2016;3:1-6. 2.Simpson K, Clin Case Rep 2021;9:e04887. 3.Jahan-Mihan A, et al. Nutrients 2011;3(5):574-603. 4.Sucher KP, Nutr Clin Pract 1986;1(3):146-150. 5.Alexander DD, et al. World J Gastrointest Pharmacol Ther 2016;7(2):306-319. 6.Mostafa MS, et al. Annals of Pediatric Surgery 2021;17:41. 7.Smith C, et al. J Clin Nutr Diet 2021;7(3):1. 8.Ibrahim H, et al. Arch Med Sci 2020; 16 (3): 592-596. 9.Erskine J, et al. J Pediatr 1998;132(2):265-269. 10.Salomon SB, et al. J Am Diet Assoc 1988;98(4):460-462. 11.Bach AC, et al. J Lipid Res 1996;37(4):708-726. 12.Bartle J, et al. Int J Nutr 2022;7(2):1-11. 13.Ford K, Gilbertson H. Int J Nutr 2022;6(4):35-45. 14.Fried MD, et al. J Pediatr 1992;120:569-572. 15.Elia M, et al. Aliment Pharmacol Ther 2008;27(2):120-145. 16.Roberfroid MB. Crit Rev Food Sci Nutr 1993;33:103-148. 17.Gibson GR, Roberfroid MB. J Nutr 1995;125(6):1401-1412. 18.Roberfroid MB, Delzenne NM. Annu Rev Nutr 1998;18:117-143. 19.Nutrition Support Interest Group. Dietitians Association of Australia (DAA), 2015. 20.Clemens RA, et al. 2002 21.Khoshoo V, et al. J Pediatr Gastroenterol Nutr 1996;22(1):48-55. 22.Dylewski ML, et al. ASPEN Clinical Nutrition Week 2006. 23.Turck D, et al. 2016 24.O'Connor G, et al. J Hum Nutr Diet 2024;1-8. 25.Thornton-Wood C, Saduera S. J Neonatol Clin Pediatr 2020;7:049. 26.Griffin D, et al. J Neonatol Clin Pediatr 2021;8:084. 27.Simpson K, J Neonatol Clin Pediatr 2021;8:079. 28.Saduera S, et al. Abstract presented at ESPEN 2024. 29.Minor G, et al. Clinical Nutrition ESPEN 55 2023;392-399. 30.Lionetti P, et al. Expert Rev Gastroenterol Hepatol 2023;17(7):665-675. 31.Giannini EG, et al. Nutrition 2006;22(3):334e42. 32.Takahashi H, et al. J Nutr Sci Vitaminol 1994;40(3):251e9. 33.Cummings JH, et al. Lancet 1978;1(8054):5e9. 34.Takahashi H, et al. Nutr Res 1993;13:649e57. 35.Pylkas AM, et al. J Med Food 2005;8(1):113e6.










