Tube feeding doesn’t have to be scary
Tube feeding is a way of getting nutrition through a tube by using a liquid form of diet.
Healthcare professionals suggest that tube feeding should be considered when a child is unable to meet his/her individual nutritional requirements and takes more than 3 hours to eat per day.1-3
The decision-making process is very complex, and we encourage you to communicate with your healthcare professional to better understand and adapt to your child’s nutritional needs.
Tube feeding can be a temporary solution until your child gets better and gains weight, or it can be a permanent solution, depending on your child’s needs. Remember that sometimes, even if your child may be able to eat, tube feeding would still be recommended to ensure he/she is getting all of his/her nutritional requirements.
The decision to start tube feeding does not usually need to be made quickly. You will be given time to consider different options and to evaluate the pros and cons of including tube feeding in your daily routine.
There are different locations and routes through which a feeding tube can be placed.
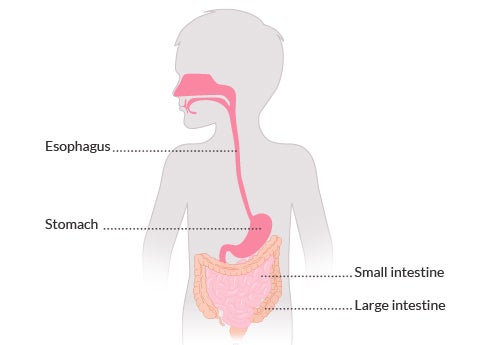
Below is a brief summary of the different tube feeding routes:4
NG and NJ tube feeding
Nasogastric and Nasojejunal tube feeding.
These form of feeding include a tube that passes through the nose, down the throat and oesophagus and then into the stomach (NG) or small intestine (NJ).
It may seem scary and troubling at first. But, with time and experience, you will get the hang of it and feel confident that your child is getting the right amount of nutrition and maintaining a healthy weight. You will also reduce feeding time dramatically, relieving so much of the stress and frustration involved with feeding. This will free up more time for other daily activities with your child.

→Click on this link to watch the full video in our real stories section
PEG and PEJ tube feeding
PEG:
The feeding tube is inserted through the skin directly into the stomach. The technical term of PEG is: Percutaneous Endoscopic Gastrostomy.
PEJ:
The feeding tube is surgically inserted into the middle section of the small intestine (the jejunum). The technical term of PEJ is: Percutaneous Endoscopic Jejunostomy.
At first, this may seem very invasive and frightening. However, you can think of PEG/PEJ- tube feeding as an umbilical cord.
Inspired by Miriam, Yehoshua’s mum
Your child is getting all of his/her nutrition through this lifeline.
These forms of feeding are very discreet and convenient, as you can feed anywhere quite easily. It is a quick, safe and reliable form of feeding that allows you to track the amount of food and hydration your child is receiving.

→Click on this link to watch the full video in our real stories section
There are different ways to deliver tube feedings and different types of feeding schedules, depending upon what your doctor has prescribed for your child.
Nutrition can be delivered continuously or in multiple deliveries (intermittent nutrition).
Continuous nutrition can be done by gravity or using a pump.4
- By gravity : A bag filled with formula or the pack of the formula hangs above the child to let the formula drip down into the tube and then into stomach. Roller clamps can be used to control the rate of flow.

- Pump Feeding: A feeding pump can be programmed to run at whatever times and feeding rates you choose to deliver bolus feedings. Make sure your healthcare professional demonstrates how to use the pump before you go home.
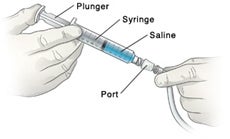
Intermittent nutrition can be done by gravity, using a pump or using a syringe.
- Intermittent feeding is a type of tube feeding that provides a certain amount of formula over a short amount of time (usually 30-60 minutes), and is typically provided several times per day.
- With a syringe: formula is poured into the syringe, then the plunger is used to push the food directly into the tube.
It may be difficult to understand now, but as you gain more experience, tube feeding can and will become second nature.1 Even though your child is being tube fed, being included in family mealtime and social events that involve food is just as important for your child as it is for you and your family.1 Speaking about tube feeding with your child will help alleviate any confusion and will allow your child to feel more reassured and comfortable during mealtime.1
There is also a wide range of formulae to choose from.
Each formula is adapted to a child’s specific needs (e.g.: caloric content, fibre content, mineral content, etc.), and some are even made with ingredients from real food!
Click on the Types Of Formulae section to better understand the different types of formulae available for feeding.
As you continue to tube feed your child at home, it’s natural to have questions, or to need some help. Your child's healthcare team can help you answer questions such as: 4
- What can I expect from the tube feeding experience and the different tube feeding options available?
- What type of equipment is needed and how do I set it up?
- How do I know if my child is getting enough nutrition?
- How do I know my child is having feeding intolerance?
- Can my child be experiencing allergic reactions?
Mealtime is an important opportunity for socialisation and development, and a part of life that children should be involved in and enjoy from an early age. Even though your child is being tube fed, being included in family mealtime and social events that involve food is just as important for your child as it is for you and your family.4
Your child's healthcare team is there to make sure that your home tube feeding experience, for you and your child is as comfortable and problem-free as possible.4
If your child is being tube fed and not taking anything by mouth, it is important to maintain oral stimulation. This is a normal part of feeding and promotes growth and development. It allows a younger child to develop skills for eating and swallowing, and helps an older child who has already learned these skills to maintain them while they are being tube fed.
Talk to your child's healthcare team for ideas about providing your child with safe opportunities to chew or suck.
When people ask when your child is going to stop using a tube to eat, it’s fine to say, “We don’t know.” For now, the focus can be on the immediate goals. Learning how to master a set-up technique. Transitioning from one type of formula to another. Growing stronger and taller every day. Thriving!
We advise you to speak with your child's healthcare team for guidance on managing feeds away from home, based on how your child is being tube fed and the feeding schedule. Your healthcare team will also help you to create a feeding plan for your child if they are attending school.
With tube feeding, there are many markers of progress! “Wins”—both big and small—are worth celebrating.4
→Click here to better understand the different types of formulae available for feeding
References:
- Romano C et al. European Society for Paediatric Gastroenterology, Hepatology and Nutrition Guidelines for the Evaluation and Treatment of Gastrointestinal and Nutritional Complications in Children With Neurological Impairment. J Pediatr Gastroenterol Nutr. 2017;65(2):242-264.
- Penagini F et al. Dietary Intakes and Nutritional Issues in Neurologically Impaired Children. Nutrients.2015;7(11):9400-15.
- Sullivan PB. Gastrointestinal disorders in children with neurodevelopmental disabilities. Dev Disabil Res Rev. 2008; 14(2):128-36.
- https://www.nestlehealthscience.us/mytubefeedingkid