Food allergies and non-allergic food hypersensitivities in babies and young children can present a real challenge. Until a diagnosis is reached, the process for parents, children and healthcare professionals can be a long and painful one.
Non-allergic food hypersensitivities, such as intolerances, arise because the body is unable to digest or reacts to certain naturally occurring component of foods, i.e., lactose or fructose, or, less commonly, food coloring, additives or preservatives. Non-allergic food hypersensitivities do not involve the immune system and are much more common than food allergies.
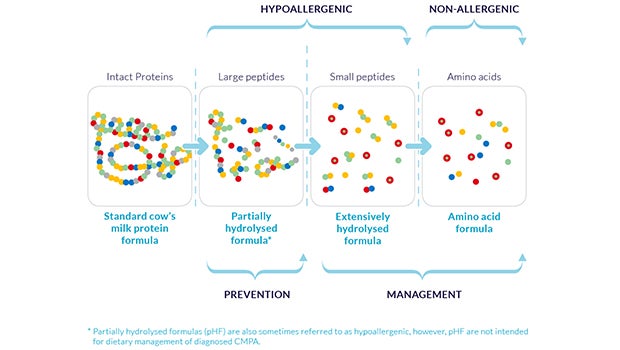
Food allergies arise due to the body’s immune system reacting to certain, normally harmless, allergy-triggering substances (allergens) in food. These allergens are almost always proteins. Proteins are one of the essential nutrients that make up the body, together with vitamins, minerals, carbohydrates and fat. Other components in food, such as lactose and sugar, do not act as allergens.
Certain allergens cause more reactions than others. Here are the top eight allergens accounting for approximately 90 percent of all allergic reactions to food in children.

The prevalence of food allergies, especially in the first years of life, has increased dramatically in the last 10 years or so. The challenge to find better ways to prevent and manage food allergies is a pressing one.
Cow’s milk protein allergy is one of the most common food allergies in children
Although cow’s milk protein is one of the most common food allergens in babies and toddlers it can be difficult to diagnose. Cow's milk protein allergy occurs when a baby’s immune system reacts negatively to the proteins in cow’s milk. If breastfed, the reaction is to the cow’s milk protein ingested by the mother and passed to the child through the breast milk, and if formula-fed, the reaction is to the milk protein in the formula. In both cases the body’s immune system sees these proteins as foreign and in an effort to protect itself, the body releases natural substances, such as histamines, which cause the allergic symptoms that your baby might be experiencing.
Cow’s milk protein allergy generally occurs for the first time between the third and fifth month of life in affected children, but can also develop later in life.
Lactose intolerance is not the same as cow’s milk protein allergy.
Cow’s milk protein allergy and lactose intolerance are often confused. Although some symptoms such as diarrhea, are similar, lactose intolerance is an inability to digest the lactose found in both cow’s milk whereas cow’s milk protein allergy is an immune reaction to certain proteins within these milks. Lactose intolerance is extremely rare before 3 years of age, even in those with cow’s milk protein allergy. After all, breast milk naturally contains a high amount of lactose.