KEY FACTS ABOUT COW’S MILK PROTEIN ALLERGY

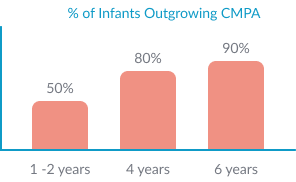
The majority of children outgrow CMPA: 50% children outgrow CMPA by 1-2 years, this increases to 80% before the age of 4. 90% of CMPA resolves by 6 years of age.1,3
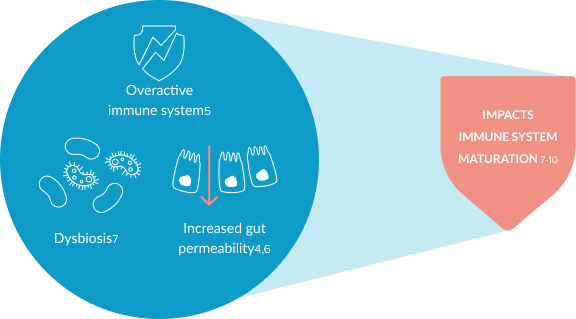
CMPA is an immune-mediated disease. It is associated with an overactive immune system, increased gut permeability and dysbiosis, which might affect the maturation of an infants’ immune system.4-10 This can lead to an increased risk of infections and future allergies.11-13